Root Canal Therapy (Endodontics) in East Gosford, Central Coast, NSW.
Our experienced team of dentists in East Gosford are committed to providing you with quality dental services on the Central Coast.
Root canal therapy is a treatment used to repair teeth where the pulp (nerve) has become infected, usually due to tooth decay or trauma. Root canal therapy can relieve dental pain and save your natural tooth. At VC Dental you can expect a comfortable experience during and after your procedure.
Call us today to discuss your dental needs, or click this button to book an appointment online now.
Root canal therapy is a treatment used to repair a tooth where the pulp (nerve) has become infected, usually due to tooth decay or trauma.
It is an often straightforward procedure that will relieve dental pain and save the natural tooth.
Root canal treatment involves removing the infected pulp and replacing it with a synthetic substitute. After the procedure the strength and original appearance of the tooth will be restored using a filling or dental crown.
Once the treatment is completed, the tooth will continue to remain healthy and functional. However, it will no longer feel sensation such as temperature (hot and cold) or pressure.
What is endodontics?
Endodontics is the area of dentistry that focuses on treating the inside of the tooth. This includes the pulp (the tissue at the centre of each tooth that contains nerves and blood vessels) and the tissues surrounding the roots of a tooth.
Why is root canal treatment necessary?
Root canal treatment is necessary when the pulp of a tooth becomes infected. This treatment allows us to save the natural tooth, rather than extracting it.
The pulp can become infected if the harder outer layers of the tooth are damaged due to decay or trauma, as it exposes the interior of the tooth to bacteria.
Once the pulp becomes infected, it loses its ability to fight the spread of the infection.
The aim of a successful root canal treatment is to remove the bacteria and prevent it from getting back into the tooth.
If the infection is left untreated it can spread into the surrounding bone. Abscesses (pus-filled pockets) may then form at the root(s) of the tooth (‘apical foramen’), and there may be localised bone loss in the jaw around the ends of the infected root canal(s).
The tooth will continue to be weakened by the bacteria and may break down completely. Eventually the tooth will need to be extracted (removed).
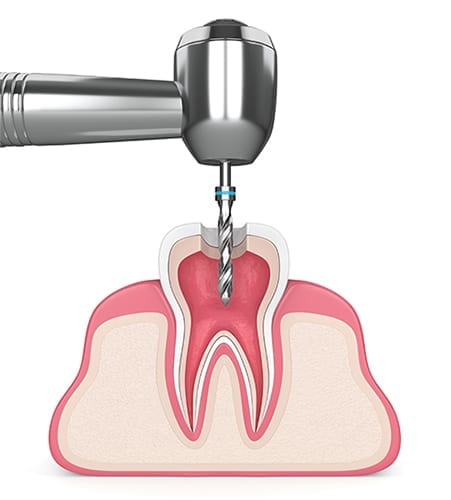
What is the procedure for root canal treatment?
Root Canal treatment involves removing the infected pulp and replacing it with a synthetic substitute. The procedure is generally completed over three appointments.
- Firstly, the dentist will drill into the tooth to access the pulp chamber. The infected pulp, along with any decay, is carefully removed.
- A very fine spinning file is then used to clean and shape the empty root canals. The inside of the tooth (including the root canals) will then be disinfected and flushed out to remove any remaining bacteria and debris.
- Then a synthetic material called gutta percha will be inserted into the root canals to fill in the space.
- The final step is to seal the tooth and restore its structural integrity and original appearance. The type of restoration required will depend on the amount of structural damage to the tooth, but may include composite resin, a dental crown, or a dental crown with a post and/or core.
1: Decayed tooth with infected pulp

2: Opening made in tooth

3: Infected pulp is removed and the canals are cleaned

4: Canals are sealed with filling (gutta-percha)

5: Opening sealed with composite filling

6: Final restoration complete
Does root canal treatment hurt?
Contrary to what you may have heard, or ‘jokes’ you may have read, modern root canal treatment is very similar to having a routine filling. The treatment is straightforward and is carried out using local anaesthetic. You can expect a comfortable experience during and after your procedure.
For nervous or anxious patients we also offer a range of sedation options if desired, which you can read about here.
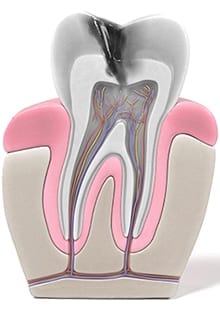
What causes the pulp infection?
Infection occurs when bacteria begin to grow in the dental pulp.
Bacteria can enter the pulp if the harder outer layers of the tooth are damaged and leave the soft interior exposed.
Reasons for this damage can include:
- A large or deep area of tooth decay
- Decay beneath an existing filling (especially if it is a deep filling)
- Decay beneath an existing restoration (for example a dental crown)
- A fracture, crack or chip in the tooth (which can have a number of causes including trauma, or habitual teeth grinding which is also known as ‘bruxism’).
- A blow to the face which may bump the tooth or cause it to become loose in the socket (for example a sporting injury).
- Advanced, untreated gum disease (periodontitis)
It’s important to note that sometimes this damage can be too minor to detect with the naked eye, so you may not know it is even there. That’s why it’s so important to attend your regular dental check-ups, so we can detect and prevent problems in their early stages.
An untreated pulp infection may also spread into the surrounding bone, forming an abscess at the end of the tooth root. As the body’s immune system reacts to the infection, it sends white blood cells to the area to try and eliminate the bacteria. Pus includes a mixture of live and dead white blood cells. When there is no way for pus to drain, it forms an abscess.
How untreated tooth decay can lead to pulp infection:
What are the symptoms?
It is important to note that in some cases there may be no pain or other symptoms present.
However, general symptoms include:
- A dull or throbbing toothache that is often spontaneous
- A toothache bad enough to wake you from sleep at night
- Severe tooth pain upon chewing or the application of pressure
- Increased and prolonged sensitivity or pain to hot and cold temperatures (which lingers for a long time after the temperature has been removed from the tooth)
- Discolouration of the tooth (it will darken)
- Swelling and tenderness of the gums near the tooth
- A recurring or persistent pimple on the gums
- An obvious cavity (damage to the tooth which may look like a hole)
- A bad taste or smell in your mouth
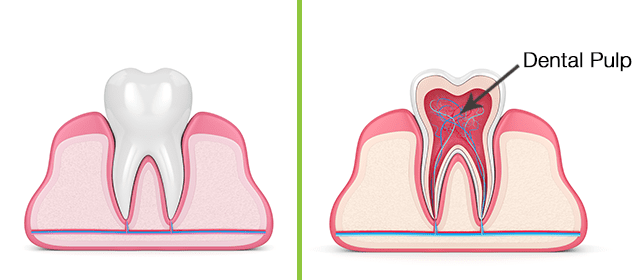
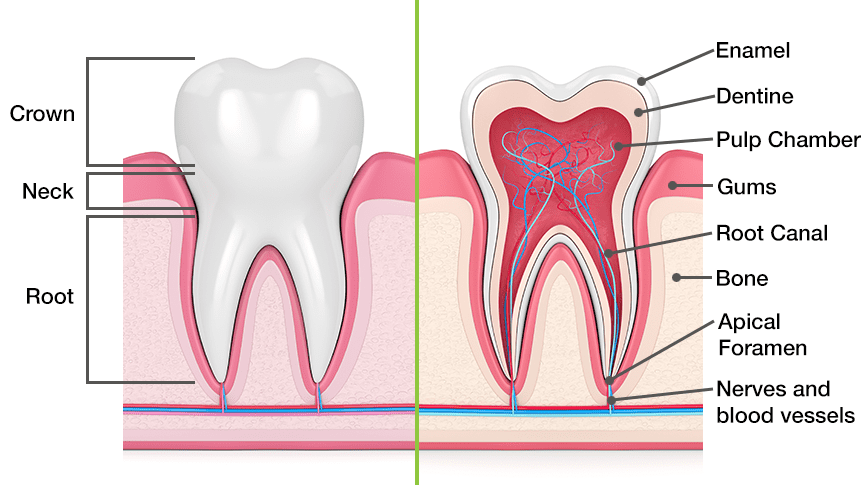
Tooth structure
A tooth has two anatomical parts. The crown is the visible part of the tooth which is covered in a protective layer of hard enamel. The root is the part of the tooth below the gum line. Generally front teeth will have only one root, whereas back teeth generally have up to three. Within each root, there can be multiple canal spaces.
The inside of a tooth is largely made out of dentine. The hollow centre of a tooth is called the pulp chamber, which contains the pulp. The pulp also extends down from the pulp chamber into and through the root canals. The pulp is made up of the nerve, blood vessels and connective tissue.
What is the pulp in a tooth and what does it do?
Dental pulp is the soft tissue in the inside of your tooth, extending from the pulp chamber to the roots.
The pulp is the ‘lifeline’ of the tooth. It keeps the tooth alive, and provides feeling and sensation to the tooth, such as temperature, pressure and pain.
The pulp contains:
- Blood vessels to supply blood and nutrients to the tooth to keep it alive
- Nerves to enable the tooth to sense pressure and temperature (hot and cold)
- Small lymph vessels carrying white blood cells to the tooth to help fight bacteria
- Connective tissue
The main function of the dental pulp is to regulate the growth and development of the tooth during childhood.
Can a tooth survive without the pulp?
If the tooth has finished growing, yes.
The pulp plays a significant role in the healthy growth and development stages of the tooth during childhood.
However, by the time we reach adulthood and the tooth has erupted through the gums and is fully mature, the pulp is not vitally important to the tooth’s health or survival.
Once the tooth is fully formed it will receive nutrition and nourishment from the tissues surrounding the root. Therefore the absence of the pulp will not affect the day to day functioning of the tooth.
The most noticeable difference will be the removal of the nerve, after which the tooth will no longer feel the sensations of pressure or temperature (hot or cold). This might take some getting used to but it will not negatively affect the functioning of the tooth.
Advantages of saving the natural tooth with root canal treatment
We always recommend root canal therapy over an extraction as it is best practice to retain the natural teeth wherever possible. A tooth that has been treated with root canal therapy can last a lifetime if good oral hygiene is practised.
There are many advantages of saving the natural tooth instead of having it extracted, including:
- Maintain normal biting force and sensation. This will ensure efficient chewing function and prevent any negative impacts on diet.
- Prevents tooth shifting causing malocclusion (‘bad bite’) and also protects other surrounding teeth from excessive wear and strain.
- Prevents bone deterioration in the jaw.
- Maintain natural appearance and prevent ‘sagging’ of the face.
However, if an extraction is required we recommend replacing the tooth rather than leaving a gap, to prevent or greatly reduce the consequences explained above. The superior replacement choice is a dental implant, however we are also able to replace teeth with bridges (tooth or implant supported), or dentures.
How can I prevent the need for root canal treatment?
You can reduce your risk of needing root canal therapy (and other dental procedures) in the future by ensuring you practise good oral hygiene daily. This includes brushing twice per day, flossing daily, and eating a healthy diet. It’s also important to attend your regular preventative care appointments so any problems can be detected and treated in their early stages.

Detailed root canal procedure information
If you would like more detailed information about the steps involved in a root canal therapy procedure, read on below.
The procedure is generally completed over three appointments:
- Firstly the infected nerve and pulp is removed (Extirpation)
- Then the canals are measured and cleaned of old debris (Mechanical Preparation)
- Lastly the canals are sealed (Obturation).
Isolation explanation:
During your appointments (mainly the second and third) the tooth will be isolated using a rubber dam (also called a ‘dental dam’). A rubber dam is a thin rectangular sheet of latex rubber, used to isolate one or more teeth from the rest of the mouth (if you are allergic to latex we have non-latex versions available). Isolating the tooth has a number of purposes:
- To prevent the bacteria in saliva from coming into contact with the tooth and therefore re-contaminating it.
- It keeps the tooth surface dry and ensures a clear view for the dentist.
- Prevents water and solutions (such as bleach) used in the procedure from entering your mouth and throat.
- Protects your throat from particles of tooth debris, and prevents instruments from accidentally entering the mouth.
- Helps prevent your gag reflex being triggered.
- Protects lips and cheeks by keeping them shielded.
Be assured you can still breathe and swallow normally with a rubber dam in place.
To place the rubber dam, a hold puncher is firstly used to make a hole in the sheet so it can fit around the tooth. The sheet is put onto a metal frame to assist in placing it, and is then stretched over the tooth (so the tooth sticks out through the punched hole). A small metal clamp is then placed around the tooth to prevent the dam from slipping and to create a water-tight barrier.

Appointments:
First appointment (Extirpation)
Extirpation is the removal of the infected pulp from the tooth. The dentist will drill an opening in the tooth to access the pulp chamber and root canal(s). An x-ray will be taken to confirm the root canal(s) have been correctly located. Then the pulp tissue (including the nerve) is carefully removed using a small instrument called a broach. The inside of the tooth is disinfected and flushed out to remove bacteria and debris. Anti-bacterial and anti-inflammatory medication is placed inside the tooth for both pain relief and to start sterilising the tooth. A temporary filling is then placed to seal the hole – keeping the medication in and any further bacteria out.
Second appointment (Mechanical Preparation)
Also called ‘instrumentation’, this appointment involves measuring the root canal lengths and then thoroughly cleaning them out (debriding).
Firstly, the temporary filling is removed and the tooth is re-accessed through the opening.
Measuring the root canals:
Measuring the root canals is important to ensure they are thoroughly cleaned and that no infection or bacteria will remain in the tip (end) of the canal. These measurements are also used to determine the amount of synthetic filling material needed to replace the pulp later on.
There are two tools used to measure the root canals: x-ray images and an electronic instrument called an apex locator.
The root canal lengths will be calculated to what is known as the ‘working distance’ (distance from the ‘apex’ – ends of the root). This needs to be calculated for all the canals in the tooth as their lengths will vary.
Cleaning the root canals:
After the canal lengths have been calculated they need to be cleaned and shaped to those measurements. Cleaning the root canals is necessary to remove as much bacteria, and remnants of decayed tissue, from the tooth as possible.
The process requires ‘chemo-mechanical preparation’, meaning it requires chemical action in the form of dental bleach (sodium hypochlorite), and mechanical action in the form of filing.
For the mechanical preparation, a combination of hand (manual) and rotary (electric) files will be used.
During the chemical preparation, the canals will be disinfected and flushed out to ensure all bacteria is removed. Because the root canal structure is made up of a system of interconnecting smaller canals (rather than just one or two main canals), using files alone would not be sufficient. The dental bleach is essential to disinfect areas that the files cannot reach.
The canals will then be dressed with an anti-bacterial solution of calcium hydroxide. This paste has a very high pH to kill off any remaining bacteria in the canal, before the final appointment to seal the canals.
At the end of this appointment the temporary filling will be replaced.

Third appointment (Obturation)
Obturation involves filling and sealing the root canal(s) completely with an airtight synthetic sterile material called gutta percha. Sealing the canals before placement of the final restoration is important to prevent them from becoming re-infected with bacteria.
The temporary filling is removed and the tooth is re-accessed through the opening.
The rubber-like root filling material (called gutta percha) is used to fill the canals. This is a thermoplastic material (‘thermo’ meaning heat and ‘plastic’ meaning shape) that is heated and then compressed into and against the root canal walls to seal them.
The gutta-percha is used in combination with an adhesive cement called a root canal sealer. The sealer is utilised as a lubricant and binding agent to eliminate any spaces within the canal where the gutta-percha may not be able to penetrate.
The temporary filling will then be replaced until the final restoration is cemented.

Final Restoration
The final step involves sealing the tooth and restoring its structural integrity, function and original appearance. The type of restoration required will depend on the amount of structural damage to the tooth, but may include composite resin, a dental crown, or a dental crown with a post and/or core.
To find out more about composite restorations, please click here.
To find out more about dental crowns, please click here.

Please note, any surgical or invasive procedure carries risks. Before proceeding you should obtain personal advice from an appropriately qualified health practitioner.


