Dental Checkup and Clean in East Gosford, Central Coast, NSW.
Our experienced team of dental hygienists in East Gosford are committed to providing you with quality dental services on the Central Coast.
At VC Dental our main focus is on preventative dentistry, which is the practise of caring for your teeth and gums to keep them healthy. Our dental hygienists can effectively treat, manage and maintain your oral health, which in turn supports your overall health.
Call us today to discuss your dental needs, or click this button to book an appointment online now.
As they say, prevention is better than cure. We want to help you keep your natural teeth for life.
Through regular oral hygiene cleans and assessments we can effectively treat, manage and maintain your oral health, which in turn supports your overall health.
What does an oral hygienist do?
A dental hygienist’s role involves treating, managing and maintaining your overall oral health. Their main focus is on preventative dentistry, which is the practice of caring for your teeth and gums to keep them healthy. This helps to avoid or lower your risk of future dental problems and other health complications.
At your oral hygiene appointments, our dental hygienists will provide a number of services including:
- Completing a full dental assessment, to note your current dental condition and detect any potential problems.
- Completing periodontal charting, to measure the health of the gum and bone levels surrounding each tooth.
- Performing professional teeth cleans. This involves scaling and polishing to remove plaque and calculus from the tooth surfaces, including between the teeth and below the gumline.
- Fluoride application
- Preventing and treating gum inflammation (gingivitis).
- Assessing, and if necessary managing, gum disease (periodontitis)
- Oral cancer screening (in conjunction with your dentist)
- Saliva testing
- Preventative treatments such as fissure sealants
- Oral health education and dental product education (including how to brush and floss your teeth properly at home).
- Advising if you should be using any specialty dental products (such as high-fluoride toothpaste, or antiseptic mouthwash) depending on your personal medical and oral condition(s).
- Advising on lifestyle and medical factors that may negatively affect the health of your mouth.
- Diagnosing any problems, or potential problems, in their early stages.
- Creating a personalised oral hygiene plan for you, which will include routine dental check-ups and a custom home-care procedure.
Maintaining good dental hygiene can greatly reduce your risk of developing cavities (tooth decay), gum disease, enamel erosion, periodontitis, and other dental problems. This equates to less dental visits, less invasive treatment, and less cost.
Tooth decay and gum disease are the two most common causes of tooth loss in adults, and they are both preventable with routine dental care and a good at-home oral hygiene routine.
Oral health and overall health
Your oral health and overall health are connected.
Poor oral hygiene can not only lead to dental decay and gum disease, but studies are showing that poor oral health is significantly associated with other chronic systemic diseases1.
Your mouth contains a balance of both good and harmful bacteria. Regular brushing, flossing and professional cleans help to reduce and remove the harmful bacteria. On the contrary, poor oral hygiene can lead to an overgrowth of harmful bacteria. Poor oral hygiene also leads to inflamed and bleeding gums, which can allow the harmful bacteria to enter into your bloodstream and affect other parts of your body.
Some conditions that may be linked to poor oral health include:
- Cardiovascular disease
- Respiratory disease
- Stroke
- Kidney disease
- Osteoporosis
- Cancer
Regular oral examinations have also become increasingly recognised as a window into the general health of the body. Research shows that a number of systemic conditions have oral manifestations (symptoms)2 meaning your dentist may be able to detect the early signs of a disease, for example oral cancer and diabetes.
Oral health and Diabetes
If you have diabetes, you are already at an increased risk of developing gum disease. However research has suggested that chronic gum disease may also make diabetes more difficult to control. The infection may cause insulin resistance, which disrupts blood sugar control3.
References
- Dental health services Victoria: Links between oral health and general health – the case for action (2011).
- Oral Manifestations of Systemic Disease – Medical University of South Carolina – Am Fam Physician (2010).
- Periodontitis and Insulin Resistance: Casual or Causal Relationship? – Diabetes & Metabolism Journal – (2012).
Clean teeth
During an oral hygiene appointment you will receive a professional teeth clean.
Your dental hygienist will remove plaque (dental biofilm) and calculus (tartar) from the surface of your teeth and around the gum line. They will also polish your teeth to remove surface staining and produce a smooth and shiny finish.
Ensuring that your mouth is free from dental plaque and calculus is the best way to prevent tooth decay and other dental problems.
Guided Biofilm Therapy
To remove plaque (dental biofilm) we use our AIRFLOW® ONE machine to perform Guided Biofilm Therapy.
Guided Biofilm Therapy is the latest technique in preventative dental care, which removes dental plaque more effectively and more comfortably than traditional cleaning methods. It greatly reduces the need to use traditional ultrasonic (electric) or hand (manual) instruments during teeth cleaning treatments, and it reduces direct contact with dental instruments.
This technology is also the “gold standard” in maintenance for patients with dental implants, or patients who are undergoing orthodontic treatment (wearing braces/brackets).
Guided Biofilm Therapy involves applying a harmless dye to the teeth to physically stain the bacteria, which will then be effectively removed with the advanced AIRFLOW® ONE handpiece.
To read more about the AIRFLOW® ONE and Guided Biofilm Therapy, please click here.
Why are dental cleans so important?
More than 500 species of bacteria have been detected in the human mouth. Within these species there are a mix of good bacteria, neutral bacteria, and harmful bacteria.
Harmful bacteria feed on sugars (complex carbohydrates) in the food you eat to product dental plaque. Dental plaque is a sticky, colourless film that forms on the surface of your teeth and can give you that “fuzzy/furry” feeling.
If plaque is not thoroughly removed by brushing and flossing it will accumulate. When plaque accumulates, it mineralises (hardens) and turns into calculus (tartar). Calculus also traps stains on your teeth and is often a brown or yellow colour.
Calculus is so strongly bonded to the teeth that the only way to remove it is using special dental tools. You will not be able to remove it yourself at home.
If not removed from the teeth, calculus can lead to tooth decay, gum disease and periodontitis.
Fresh breath
Good oral hygiene is important for fresh breath.
During your appointment the dental hygienist will perform a range of services to help you prevent, eliminate or treat bad breath.
These include:
- Professional teeth cleaning to remove plaque, calculus and impacted food that harbour bacteria.
- Assess all surfaces of your teeth and gums for cavities (tooth decay), faulty (leaking or broken) restorations and gum disease.
- Assess your medical conditions and medications (if any).
- Discuss any relevant lifestyle factors.
- Provide you with a personalised at-home oral hygiene routine.
Bad Breath
What is bad breath?
Bad breath (also called ‘halitosis’) is characterised by a persistent, unpleasant odour emanating from the mouth.
It has many causes, however it is most commonly caused by poor oral hygiene. Other causes include medical conditions, medications, illness and lifestyle choices.
Preventing bad breath
The best way to prevent bad breath is to brush your teeth, floss, and clean your tongue daily, in conjunction with attending regular oral hygiene appointments.
At your oral hygiene appointments we not only provide preventative care (through professional cleans), but we also assess any potential underlying causes of bad breath so they can be treated. We may even refer you to your GP or specialist for further diagnosis if required.
Oral health tips to avoid bad breath
- Brush your teeth (properly) at least twice daily.
- Floss at least once daily (to remove plaque and food trapped between your teeth).
- If you wear dentures, ensure they are thoroughly cleaned daily.
- Clean your tongue either by brushing with your toothbrush or using a tongue scraper.
- Drink plenty of water through the day to keep your mouth hydrated. This can prevent a dry mouth, which causes your body to slow down the production of saliva to conserve water.
- Drink water after consuming food and drinks especially if they are sugary/sticky. This can help remove some of the residue from your teeth that bacteria would otherwise feed on and cause plaque.
- Refrain from smoking.
- Avoid food or habits that cause a diuretic affect (such as alcohol and tobacco), which can create a dry mouth environment.
- Chew sugar-free gum to increase the flow of saliva.
Poor oral hygiene
Dental plaque is a biofilm (mass) of bacteria that grows on surfaces within the mouth daily. If plaque is not adequately removed it can build up, meaning an overgrowth of bad bacteria. These bacteria are living organisms that generate gases (volatile sulphur compounds or ‘VSC’) that create an unpleasant odour.
Food that gets trapped between your teeth and is not removed also contributes to bad breath as it rots, as well as feeding the bad bacteria in your mouth.
Cavities (tooth decay) and faulty (leaking or broken) restorations can also cause bad breath as they may trap food and bacteria in your mouth.
Persistent bad breath or a bad taste in the mouth is also a common symptom of gum disease, which is an infection caused by a build-up of hardened plaque (calculus) on the teeth.
Other causes
Sometimes you can experience bad breath even if your mouth is clean and healthy. In these cases, medical conditions, medications, illnesses or lifestyle choices (or a combination of these) may be causing your symptoms. These can include:
Medications
Some medications can have a side-effect of bad breath by either causing a dry mouth, or releasing chemicals into the breath when they break down in the body. Medications commonly associated with bad breath include angina medication, high blood pressure medication, antihistamines, antidepressants and antipsychotic agents.
Dry mouth
Dry mouth (xerostomia) can be caused by medication, alcohol, stress, breathing with your mouth open or a medical condition. It may be transient (such as when you wake up in the morning after sleeping) or chronic.
Dry mouth occurs when the flow of saliva decreases, which can cause bad breath. Saliva is a natural cleanser for your mouth. It inhibits the growth of bacteria that contribute to bad breath by cleansing the mouth and removing particles that may cause odour.
Medical conditions
As well as dry mouth syndrome (xerostomia), other medical conditions that can affect the breath include diabetes, gastrointestinal diseases and liver or kidney problems.
Illnesses
Infections in the throat, nose or lungs (such as bronchitis, sinusitis and tonsillitis) as well as a cold or flu that causes post-nasal discharge.
Smoking
Tobacco products cause bad breath both from the chemicals released when burned/inhaled, and because they can dehydrate the mouth and produce dry mouth symptoms.
Smoking also causes staining, loss of taste, irritates the gums and is a common cause of gum disease.
Chronic bad breath
Chronic bad breath can be a sign that something is not right. If you are suffering from persistent bad breath, schedule an appointment with your dentist or health professional.
Healthy gums
How we keep your gums healthy
During your appointments we provide both preventative care and thorough assessment for gum disease.
This includes:
- Performing a professional clean to remove any plaque build-up on your teeth and keep your gums healthy.
- Performing a full dental assessment (periodontal charting) of your gum health and bone levels around each tooth.
- Discussing any relevant lifestyle factors or medications that could be contributing factors.
Preventing and treating gum disease so you can keep your natural teeth is one of our main priorities.
Gum disease is a serious condition and is one of the leading causes of tooth loss in adults. It is entirely preventable with good oral hygiene, however once you have gum disease in its more advanced stages it is generally not reversible (however it can be managed).
Early intervention
Attending your routine oral hygiene appointments is important so we can identify gum disease in its early stages, giving us the best chance to treat and reverse it.
Gum disease can progress slowly over time without the patient knowing they even have it (especially if you smoke). Patients may only become aware that something might be wrong when the disease has already progressed to more advanced stages.
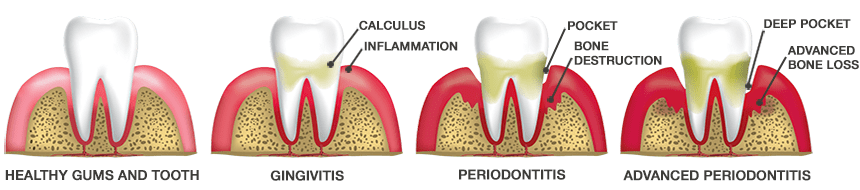
Types of gum disease
Symptoms of gum disease include inflamed, bleeding or painful gums, bad breath, loose teeth, tooth loss and bone loss.
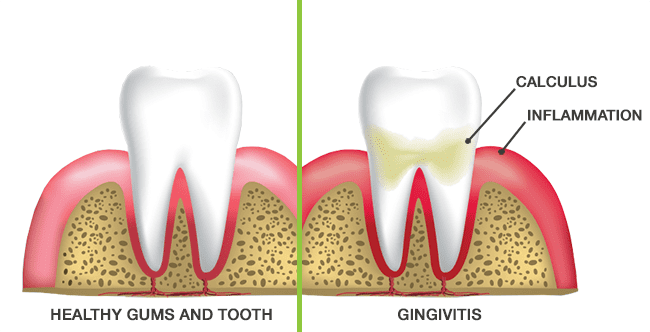
Gum disease in its early stages is called gingivitis, which is a gum infection that causes gum inflammation. At this stage gum disease is treatable and reversible.
If Gingivitis is not treated it can progress to Periodontal Disease which is an advanced form of gum disease that also affects the bone and ligaments surrounding the teeth. Periodontitis is generally not reversible however it can be actively managed through a comprehensive oral hygiene routine including regular visits to your dental hygienist.
Gingivitis
Gingivitis is caused by the accumulation of dental plaque on and between the tooth surfaces, and along the gumline. If plaque is not thoroughly removed it will harden into calculus (tartar).
This build-up of plaque and calculus contains bacteria that cause an infection in the gums called gingivitis. Gingivitis is inflammation of the gums which can include redness, swelling and irritation. A common sign of gingivitis is bleeding gums, or seeing blood in the sink when you spit out after brushing.
It is important for smokers to note that bleeding gums are often masked due to the poor blood supply to the gums.
Gingivitis is reversible and preventable through routine hygiene appointments and good at-home hygiene care.
If left untreated, gingivitis can lead to periodontitis (periodontal disease).
Periodontal disease
Periodontal disease is an infection of the gums and supporting structures (periodontal ligaments and alveolar bone) surrounding the teeth.
The gums pull away from the teeth, opening up pockets and exposing the roots of the teeth. These pockets are filled with plaque and calculus (tartar) and become a breeding ground for bacteria.
The body’s natural response to infection, and toxins from the bacteria, cause the connective tissues and bone around the teeth to be destroyed.
Advanced periodontal disease leads to sensitive teeth, loose teeth, and the appearance of elongated teeth.
Periodontitis is a serious condition that can cause tooth loss if it is left unmanaged.
Preventative treatment
Preventative dental treatments are used to keep your teeth and gums healthy.
This lowers your risk of dental problems and helps you keep your natural teeth for life.
Preventative treatment is important for adults to prevent decay, gum disease and tooth loss.
Preventative treatment is important for children so we can ensure their adult teeth grow strong and healthy, and are well cared for so they will last a lifetime.
We use a number of treatments to keep your teeth in great shape:
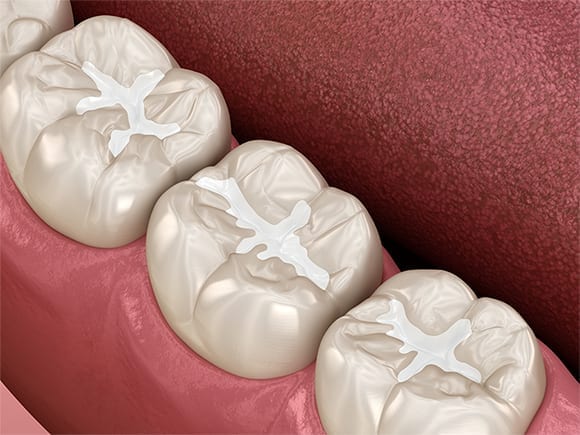
Fissure sealants
Fissure sealants are a protective layer of resin applied to the chewing surface of the back teeth (molars), to help prevent tooth decay.
Fissures are the grooves that occur on the chewing surfaces of the back teeth. Sometimes these fissures are too deep and may be difficult to clean with a toothbrush. This can lead to food, plaque and bacteria becoming trapped in the fissures and causing cavities.
Fissure sealants are made from tooth-coloured resin which flows into the deep grooves to fill them.
The sealant will act as a barrier to bacteria and food debris, and will make the tooth surface smoother and therefore easier to clean.
The application of sealants does not require any drilling or local anaesthetic, and multiple sealants can be applied in one appointment.
Plaque disclosing
Plaque can be difficult to see with the naked eye due to its light colouring when it first develops.
Plaque disclosing involves applying a vegetable-based dye to the teeth to stain plaque lingering on the teeth. This will allow you to clearly see the areas where plaque is not being correctly removed.
We use an advanced ‘Tri Plaque’ gel which shows different stages of plaque damage.
The use of plaque disclosing helps you be more aware of problem areas when brushing and allows us to help you with your toothbrushing technique.
These results are also recorded and progress is tracked throughout subsequent appointments.
Saliva testing
Saliva is the body’s natural defence system for the teeth and mouth. It is particularly important for protecting the outer tooth surface (enamel) from decay by neutralising acids caused by bacterial plaque.
In specific cases where there may be unexplained decay, a simple saliva test is used to identify, measure and assess saliva condition. This can help us manage your oral health effectively and tailor treatments and products to suit you.
Some salivary functions include:
- Neutralising acids
- Flushing food and bacteria from the mouth
- Acting as a lubricant
- Providing remineralisation to the tooth surface (enamel)
Fluoride application
Fluoride is a natural mineral found in the environment, including in food and water. It helps to strengthen teeth and prevent tooth decay, by making teeth more resistant to acid attacks from plaque and sugars.
Topical fluoride applications can be carried out at your regular hygiene appointments. This is done with a concentrated fluoride gel, which is placed in a foam tray and sits over the teeth for 1 minute.
Lifestyle factors
Your lifestyle choices have an impact (both good and bad) on the health of your teeth and mouth.
This can include the foods you eat, whether you smoke, your alcohol consumption, if you have tongue or lip piercings, how much stress you are under, and any medication you take (both prescribed and non-prescribed).
During your appointment, your hygienist will discuss your personal circumstances with you and if there are any relevant factors that may negatively impact on your oral health. They will also provide you with personal, comprehensive nutritional and dietary advice.
Diet and tooth decay
Everything you eat and drink can have a major effect on the health of your teeth and gums, particularly whether you develop tooth decay, which is a preventable disease.
Foods high in sugar and refined carbohydrates (which break down to starch and then sugar), feed the bacteria in your mouth which in turn produce acids that can attack the outer layer of your tooth (the enamel). This does not only mean processed foods; it also includes foods high in natural sugars and starches. This is known as an ‘acid attack’ and results in the demineralisation of your enamel and can cause tooth decay.
Saliva provides a natural defence mechanism to help prevent tooth decay, by neutralising the acids produced by bacteria through a process called remineralisation. Saliva also helps to wash away some of the sugar and food particles in your mouth. This ‘attack and recovery’ process occurs every time you eat and drink. However, if you frequently consume sugary food and drinks, saliva may not have time to remineralise the teeth properly after each ‘attack’.
Therefore the greater risk is the frequency in which these foods are consumed, rather than the quantity they are consumed in. By limiting snacking throughout the day, you can reduce the occurrences of ‘acid attacks’.
Drinking water throughout the day, including after meals, can also help reduce your risk of tooth decay in a number of ways. Water helps keep your mouth hydrated which can prevent a dry mouth. It also helps wash away leftover food (and sugar) residue from your teeth, as well as diluting the acids produced by bacteria in your mouth. If your local water also contains fluoride you are even helping to strengthen your teeth at the same time.
Chewing sugar-free gum, especially after meals, can also help reduce your risk of tooth decay as it stimulates the salivary glands to produce more saliva, with helps neutralise decay-causing acid attacks.
Smoking
It is well known that smoking has many negative impacts on both your overall health and your dental health.
Smoking most noticeably causes staining and discolouration of the teeth (caused by the nicotine and tar in cigarettes). It also causes bad breath, both from the chemicals released when burned/inhaled, and because they can dehydrate the mouth and produce dry mouth symptoms.
However, more seriously smoking can cause loss of taste, a decreased blood flow to the gums, bone shrinkage, an imbalance in your saliva, gum irritation, gum disease and oral cancer.
Alcohol
Frequent and prolonged consumption of alcohol can have a range of negative impacts on your overall health, but did you know it can also contribute to tooth decay?
The sugar and acidity in alcohol, especially if you mix alcohol with sugary soft drinks, cause acid attacks on your enamel when the bacteria in your mouth feed on them.
Alcohol is also a diuretic which can cause a dry mouth, preventing saliva from being able to properly remineralise your teeth from the acid attacks, and wash away the sugars from your mouth.
Compounding these issues is the fact that many people come home from a night out and go straight to bed, forgetting to brush their teeth first. This leaves your mouth unprotected from acid attacks all night.
To help reduce your risk of tooth decay if you are consuming alcohol, drink water between drinks throughout the night to help remove the sugars from your teeth and keep your mouth hydrated (which can help prevent a dry mouth), make sure you brush your teeth before you go to sleep to remove any accumulated plaque, and continue to drink plenty of water the next day after you wake up.
Oral cancer screening
Your dentist and dental hygienist will perform a comprehensive oral mucosal examination (oral cancer check) during your appointments, to look for signs of cancer or precancerous conditions in your mouth.
This is an important aspect of your preventative care appointments, as often the first signs of mouth cancer are detected by a dental professional.
The goal of oral cancer screening is to identify any symptoms early, when there is a greater chance for a cure.
Oral cancer screening comprises of both a visual and physical examination of the oral region and connected areas.
The visual examination includes looking at your face, neck, lips, gums, the inside of your cheeks, your tongue, and the roof and floor of your mouth.
The physical examination includes feeling around the head, cheeks, jaw, under your chin and in your mouth for any unusual nodules or textures, and to assess movement. You may be asked if you feel any discomfort in certain areas.
It’s important to note that oral cancer screening is a precautionary service, it’s not diagnostic. Oral cancer can only be accurately diagnosed with a biopsy (when a sample of tissue is removed and examined under a microscope).
However, we can identify any suspicious-looking areas or growths. If we see anything that causes us concern, we will refer you to a medical practitioner/specialist to have it further evaluated (and to perform a biopsy if required).
This information is intended to promote understanding of and knowledge about general oral health topics. It should not be taken as personal, professional advice; nor treatment or diagnosis. Always seek professional advice from an appropriately qualified medical practitioner.


